For our 3rd coursework, we are tasked to read a research article entitled “Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions”, then do a write-up on the following scenario:
You have been selected to be the project manager for a DOH project with the task of implementing a national EHR that all government hospitals will implement. Select at least three barriers to EHR implementation from the article that you believe to be the most important ones that might adversely affect your implementation. Explain and provide supporting cases/articles/information.

The objective of the research study as stated in the authors’ abstract was to identify, categorize, and analyze barriers perceived by physicians to the adoption of Electronic Medical Records (EMRs) in order to provide implementers with beneficial intervention options. They based their systematic literature review from different research papers from 1998 to 2009. The study resulted to eight main categories of barriers including 31 sub-categories which are the following:
A: Financial
- Start-up costs
- High ongoing cost
- Uncertainty over Return on Investment (ROI)
- Lack of financial resources
B: Technical
- Physicians and/or staff lack computer skills
- Lack of technical training and support
- Complexity of the system
- Limitations of the system
- Lack of customizability
- Lack of Reliability
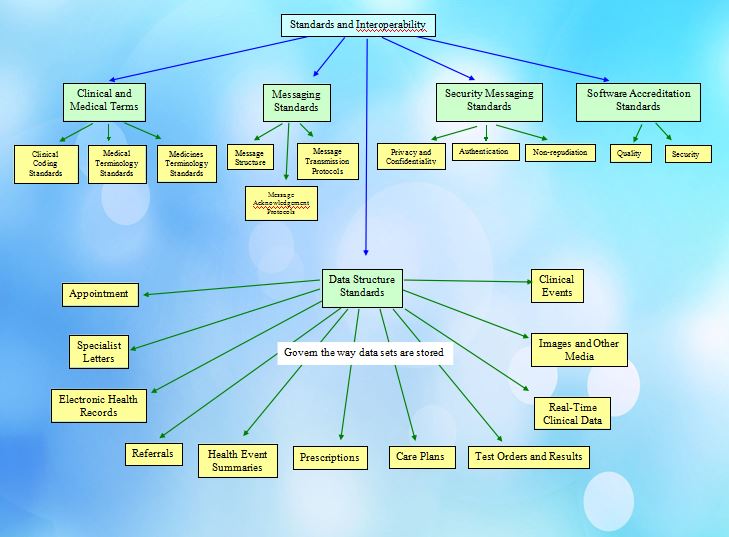
- Interconnectivity/Standardization
- Lack of computers/hardware
C: Time
- Time required to select, purchase, and implement the system
- Time to learn the system
- Time required to enter data
- More time per patient
- Time to convert patient records
D: Psychological
- Lack of belief in EMRs
- Need for control
E: Social
- Uncertainty about the vendor
- Lack of support from external parties
- Interference with doctor-patient relationship
- Lack of support from other colleagues
- Lack of support from the management level
F: Legal
- Privacy or security concerns
G: Organizational
- Organizational size
- Organizational type
H: Change Process
- Lack of support from the organizational culture
- Lack of incentives
- Lack of participation
- Lack of leadership
If I were to be the project manager who will implement a national Electronic Health Record (EHR) that government hospitals will use, part of my job is to plan on how to successfully implement this project and sorts of barriers can inhibit successful planning. To be able to achieve the desired results, I must identify all possible barriers and exert efforts to deal with them.
Though all of the identified barriers mentioned above are important, I believe that these three to be discussed below have the most impact in the EHR implementation.
1. FINANCIAL
According to a survey, the cost of installing and maintaining EHR systems is the biggest barrier to the adoption by medical group practices, particularly for the smallest physician groups. Since this is a national project implementation, as the project manager, it is essential to know the budget and all the costs included such as purchase price, coordination costs, monitoring costs, and negotiating costs, upgrade costs, and governance costs, to get the EHR implemented across all the government hospitals. A lack of financial fund can consequentially cause problems to sustain the deployment.
2. ORGANIZATIONAL
The organizational category of barrier includes the characteristics of individual practices which are a factor in EHR implementation such as the size and the type of the organization. As a project manager, I have to assess the size of the hospital because this characteristic affects the extent of support and training systems. For instance, a large organization requires more time to choose, purchase, learn a system, and gather data.
Also, this category barrier may adversely affect the implementation of EHR due to its influence to the other categories because it determines the relative significance of the other barriers even before implementation has started. For example, a small practice is foreseen to face greater challenges in dealing with financial issues, which is one of the barriers in EHR implementation, than a large practice. The lack of knowledge in this category barrier can result to other major barriers.
3. CHANGE PROCESS
EHR implementation entails acceptance from physicians to new practices, however, some physicians resist. As a project manager, the “Change Process” category must also be identified as one of the most important to be addressed as this can bring about other barriers to a successful EHR adoption process. The government hospitals should show support by building an EHR-friendly culture as part of the change process. This can be achieved by letting experienced doctors be part of the application team leaders in the project who will participate in the whole process. This will not only help the physicians accept the change enthusiastically but their involvement will also make the system tailored to the doctors’ preferred workflows. Another way to do the change process is to make certain that the management of the government hospitals are motivating the physicians by presenting the benefits they can get from the usage of EHR. The more they see the advantages, the more motivated they will be, and the more willing they will become in accepting the new process.
Electronic health records can improve the health care delivery but the process of the implementation is challenging not only on the execution but starting from the planning stage which includes identifying the barriers to the implementation. Nevertheless, these barriers can be overcome. Like what Joshua J. Marine said:
“Challenges are what make life interesting and
overcoming them is what makes life meaningful.”